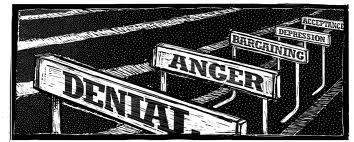
In 1969, the Swiss American psychiatrist Elizabeth Kübler-Ross published her groundbreaking book called ‘On Death and Dying’. In the book, she introduced the now famous ‘Five Stages of Grief’. Her theory suggested that there are five stages of adjustment after a loss, which are:
- Denial
- Anger
- Bargaining
- Depression
- Acceptance
The theory described the five stages of grief concerning the mourning of a loved one. However, these five stages have also been used to describe many areas that involve a loss.
These five stages of grief can also apply to a diagnosis of a chronic illness or the onset of a progressive disability. Mourning the loss of good health, the loss of a future that we may not have as a result of the diagnosis. And for the activities that we once enjoyed but which may be prevented by the symptoms of the chronic illness or disability.
[Tweet “The 5 Stages of Grief can be applicable when diagnosed with a chronic illness…”]
An example of these stages in action can be as follows:
Denial
We immediately are in denial of the new situation and cannot accept that it is true. Regarding chronic illness, we may question the doctor and ask whether he is confident that the diagnosis is correct. A request may be made for further investigations as we cannot accept the diagnosis as fact. We may also not be open to new medications or treatments suggested as that would mean the condition is real.
Anger
Like many others, anger is a normal feeling when living with chronic illness. We are angry at the illness itself due to the severe symptoms that it causes; angry at the limitations it places upon our lives; doctors who made the diagnosis as well as those who didn’t believe you. We are often angry at people around us who are still able to do all the things that we are no longer able to do. Anger is one of the five stages that those living with chronic illness reverts to, especially when symptoms are particularly severe.
[Tweet “Anger is a stage those living with chronic illness reverts to, especially when symptoms are severe.”]
Bargaining
Although anger stays for a while, we eventually progress to the third stage which is bargaining. Often, when living with a chronic illness, we become lost in a world of “What if” and “If Only” statements. We want to return to the life we had before illness, so we attempt to bargain with our bodies.
We promise that we will take all our medications correctly, and keep to a healthy diet in exchange for the condition to disappear. A promise is made to do anything in exchange for a cure and to be able to return to a normal life.
[Tweet “When living with a chronic illness we become lost in a world of “What If” and “If Only” statements.”]
Depression
As times passes; we slowly realise that bargaining isn’t working. As there is no sign of a cure or a return to our old life we begin to lose hope. Often, we slide into a depression. The depression isn’t a sign of a mental illness however but a response to the loss of our previous life. We turn inward and withdraw from life, and get stuck in a fog of sadness, despair and hopelessness.
[Tweet “As there is no sign of a cure or a return to our old life we can slide into depression.”]
Acceptance
The move into acceptance is a slow and gradual process. To reiterate it is not a state of being perfectly fine with being chronically ill but is perhaps a state in which we have more good days than bad ones.
However, this is not a single process. These five stages of grief are linear and one in which we often regress to previous steps. The need to work through them all over again, especially at times when the condition gets worse. As we worsen we return to the first stage of denial and we need to work through all the stages just like we did after the initial diagnosis. As our health deteriorates, we are essentially mourning the loss of another piece of ourselves.
[Tweet “Acceptance is about finally recognising and acknowledging the permanence of chronic illness.”]
The importance of acceptance can be brilliantly summed up by a famous quote by Joseph Campbell:
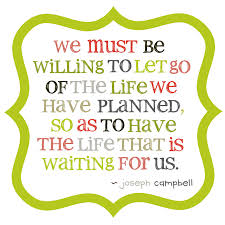
This post is about acceptance – to acknowledge the changes in our situation and declining health. It is not about being completely fine or deliriously happy about the illness or disability. Acceptance is about finally recognising and acknowledging the permanence and reality of life after diagnosis.
To learn to readjust to our new reality we need to embrace the life we have now. Acceptance is not about giving up.
[Tweet “Acceptance is not about giving up but to learn to readjust to our new reality.”]
I thought about the ‘Five Stages of Grief’ recently after a day out with my carer. As my regular readers may be aware, I have had to start using my wheelchair on a much more regular basis, especially when out for hours due to the worsening weakness in my legs.
Last week, my carer commented on how much more confident I seemed since I started using the wheelchair and how I seemed to enjoy days out much more. A reason for this is because I am in the wheelchair, I am not always on edge that my legs will give way, or on the days when the weakness is severe, I am not waiting for my legs to collapse.
However, as I also live with constant dizziness and regular bouts of vertigo and as a result of the continual movement while in the wheelchair, it was challenging for me to use it. So why do I seem so much more confident using the wheelchair than sitting down, and enjoying being out much more when it causes such symptoms?

One possibility is that as suggested by the theory discussed, I have finally accepted that I need the wheelchair. Perhaps, I have finally moved through these five stages and now accepted my new reality. Before, I became worried not only about the wheelchair’s effect on my vestibular system but also with the judgements of other people. That however no longer is a concern of mine and happy to be in the wheelchair.
Perhaps, it is much easier to live with a new situation when we have reached acceptance. We need to embrace the new reality to live life to the fullest despite any limitations that chronic illness has placed upon our lives.
[Tweet “It is easier to live life despite the limitations of living with a chronic illness when we have reached acceptance.”]